HOT
 Metal Technology (MTI) forges new path with meta…
Metal Technology (MTI) forges new path with meta… Reaching the Outer Limits with GibbsCAM and the …
Reaching the Outer Limits with GibbsCAM and the … Planetary Resources Uses 3D Printed Casting Patt…
Planetary Resources Uses 3D Printed Casting Patt… Rapid Part Replacement Ready for Take Off?
Rapid Part Replacement Ready for Take Off? Bushnell Verifies High Detail Optics Designs wit…
Bushnell Verifies High Detail Optics Designs wit… Birdstone Delivers Schweppes Redesign with 3D Sy…
Birdstone Delivers Schweppes Redesign with 3D Sy… 3D ProMetal Optimizes Next-Gen Medical Component…
3D ProMetal Optimizes Next-Gen Medical Component…
Changing the Face of Craniomaxillofacial Surgery
The Challenge
Craniomaxillofacial surgeons perform major structural surgeries that involve bones and soft tissues (skin and muscle) in the head and neck area. The complex anatomy of the craniofacial skeleton presents a challenge when attempting to achieve the ideal aesthetic and functional outcomes.
A 22 year-old female suffering from left orbital fracture after falling from the 2nd floor was admitted to the Craniomaxillofacial Surgery unit at Galilee Medical Center in Nahariya, Israel, headed by Prof. Samer Saruji. It was decided to create an implant in order to reconstruct the missing part in her left orbit.

“Due to the complexity of the fracture and its delicate location, one of the challenges the team faced was to achieve optimal fitting of the implant to the patient’s anatomy while preserving its functionality and highest aesthetic results,” said Dr. Lior Tzadok, Senior Craniomaxillofacial Surgeon, Galilee Medical Center.
The Solution
Six months ago, the institution initiated a surgical planning workflow using 3D Systems’ surgical planning software applications and a 3D printer.
“The ability to use a few products from the same company helped us achieve a faster and smoother process to the end result, without wasting time between the workflow steps,” said Dr. Adib Zoabi, Craniomaxillofacial Fellow, Galilee Medical Center.
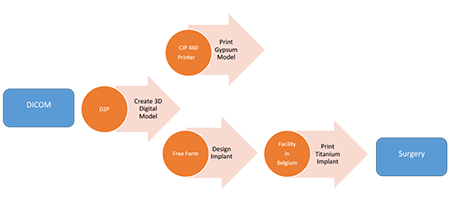
“Using D2P software, we were able to segment the replicate structures out of the patient’s CT scan and send it for printing in our 3D lab (CJP 460 printer, 3D Systems). The printed gypsum model allowed us to better understand the patient’s pathology. Using FreeForm 3D systems’ design software, we mirrored the healthy side, shaped the implant and sent the implant file to 3D Systems’ FDA and CE registered facility in Leuven, Belgium and received a Patient Specific platinum Implant (PSI),” said Dr. Zoabi.
In addition to surgical planning, the physicians used the printed gypsum model to verify the titanium implant fitting and explained to the patient and family the severity of the problem and outline the surgery plan and the expected result.
“Since the technology enables us to accurately predict and reach the result as we planned, it is now easier for us to share the surgical plan with the patient and his family,” said Dr. Tzadok.
This has also a positive effect on the patient’s understanding and trust. “The physician showed me the printed model of my healthy and fractured orbit. I didn’t realize the magnitude of the problem until I saw the fracture size. I could not understand it by looking at the CT,” said the patient. “After the physician’s explanation about the procedure and seeing the implant, I felt more confident to have the surgery.”

The Outcome
Reconstructive surgery has historically relied on the surgeon’s subjective assessment of form and aesthetics preoperatively and intraoperatively, with intraoperative decision making based on visual anatomical inspection, after bending the metal plate implant. Although good outcomes can and are often achieved, the highly subjective nature of this process results in variable surgeon-specific outcomes and can also lead to prolonged surgical time.

“The surgery was smooth and quick, and the result was beyond our expectations,” said Dr. Tzadok. “The most amazing reaction to the planning was received in the OR. Usually after the surgery, the team was examining the patient from different angles to see if we brought the eyeball to its place. We could not know if we were in the correct place until the next morning’s imaging and this kept us up all night. In this surgery, immediately when we put the printed plate in place according to planning, we were all looking and it was obvious that we have the correct positioning. The eyeballs were exactly where we planned. For surgeons, it brings something we didn’t have before, knowing the magnitude of the problem, being able to copy from the healthy side to the pathological side and to predict the outcome. This minimizes the risk of error, shortens the operation time and helps us know what will be the final product and ‘promise it’ to our patients.”
The shortened procedure time and the excellent surgical result effect on the patient was obvious. “The operation was quick and almost painless, except for a slight pain in one eye. I was released two days later. There was no scar and no one knows I had an eye operation, which is amazing. After three days, I was at home reading books,” said the patient.

The Future
Galilee Medical established a 3D printing lab in the craniomaxillofacial unit. This is the first and currently the only center in Israel that incorporated in-house end-to-end surgical planning workflow, in which physicians have the knowhow for using 3D Systems’ surgical planning applications and 3D printing.

“We are speaking in new terms in the surgical world that are different from everything we used to know. More and more ‘dry runs’ are performed before the actual surgery. The surgeon is becoming a designer,” said Prof. Samer Saruji, Head of CMF Unit, Galilee Medical. “We have just started to use this workflow in our daily practice and we already see the great progress in our patient outcome. The errors are dramatically reduced and the surgical ability of the surgeon is constantly improving. In addition, having those capabilities in-house helps us to reduce procedural cost. Our success here leads to a growing interest in the hospital to expand the 3D Lab usage to other departments, such as neurosurgery. We hope to see this trend improving patient outcomes in more and more areas,” said Prof. Saruji.